Introduction
Skin diseases are often diagnosed based on visual inspection alone. However, a variety of situations call for additional diagnostic measures which may be invasive (e.g., skin biopsy) or non-invasive (e.g., KOH preparation, nail clipping, dermoscopy). Dermoscopy has become increasingly popular over the last several decades and has become an indispensable tool for many dermatologists. While a plethora of evidence has demonstrated its utility in the diagnosis of keratinocyte carcinomas, melanocytic lesions, and inflammatory conditions,1–3 extra-diagnostic uses continue to broaden the role of dermoscopy. These include the evaluation of disease activity, enhancement of doctor-patient communication, and improvement of aesthetic outcomes.4 Given its lengthy history, modern prevalence, and growing indications, a review of the origins and current state of dermoscopy seems both relevant and worthwhile.
Origin of Dermoscopy
Dermoscopy, also known as dermatoscopy, epiluminescence microscopy, or skin surface microscopy, dates back to the renaissance period, even before the emergence of dermatology as a science.5 The basic principle is characterized by transillumination of a lesion and evaluation of its microscopic features under magnification.6 With the use of this technique, Pierre Borel pioneered an early version of dermoscopy and published “De vero telescopii inventore” in 1655 and “Observationum microscopicarum centuriae” in 1656. At this time, the primary use involved evaluation of capillaries in the nail bed.5,7 While the technique was reproduced eight years later by Johan Christophorus Kolhause,5,8 a gap of nearly 200 years took place before further reports of this technique arose in the literature.
In 1893, Paul Gerson Unna published a novel paper entitled “Diaskopie.”9 He studied the refractive nature of the epidermis and determined that skin could be made more translucent with water soluble oils, which allow for the natural polarization of light. Unna demonstrated that oils can be used with the concept of Brewster’s angle (defined as the incident angle at which polarized light transmits through a surface with no reflection) to transmit light through the skin’s surface, illuminating a lesion. Thus, the use of immersion microscopy allowed for sharper, brighter, and deeper visualization of lesions, without the limits imposed by reflected light.10,11 As this technique matured, the term “dermatoscopy” was introduced in the 1920s, following several publications by Johann Saphier.12,13 At this time, dermoscopy was primarily used for the evaluation of capillaries under normal and pathological conditions. Additionally, Saphier described criteria for discriminating between cutaneous tuberculosis and syphilis, an important matter at the time.5 Although Saphier did not thoroughly investigate features of benign versus malignant melanocytic lesions, he did study melanocytic nevi and coined the term “pigment cells,” which continues to be used today. Dermoscopy was first adopted in the U.S after a Houston dermatologist, Jeffrey Michael, published a paper describing the technique in 1922.14
A period of time passed before Lean Goldman began publishing his studies in the 1950s, describing the utility of skin microscopy in the evaluation of benign and malignant melanocytic lesions.15–17 While he noted several defining pigmentary features, his studies were hindered by devices which yielded inadequate illumination and detail. However, advancements in the quality of dermatoscopes, along with the work of Ronald Mackie in the 1970s, marked a turning point in the history of modern dermoscopy. Mackie was able to differentiate between malignant and nonmalignant pigmented lesions with precision and accuracy.18 Throughout the 1980s, further refinement of the technique led to additional publications and in 1989, the first Consensus Conference on Skin Microscopy in Hamburg, Germany, was held to standardize the terminology of morphologic features.19 In the same year, a team of physicians led by professor Otto Braun-Falco in collaboration with Heine Optotechnik, developed a hand-held dermatoscope illuminated by a halogen lamp, known as the Delta-10 (Fig. 1).20 While immersion oil continued to be used to polarize light and reduce reflection, the convenience of this dermatoscope aided in the rapid diagnosis of pigmented skin lesions,20 leading to increased popularity of the technique throughout the 1990s.
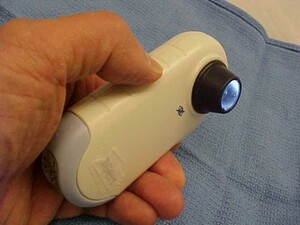
Following this rise in popularity, a handheld dermatoscope known as the DermLite, was patented in 2001. This dermatoscope featured polarized illumination coupled with a cross-polarized viewer (Fig. 2), allowing for visualization of deeper skin structures without the use of immersion oil or direct skin contact, both of which were known to distort the appearance of skin structures.21 The first generation DermLite was the first of its kind and gave rise to the modern dermatoscope.
Use of Dermoscopy in the 21st Century
In 2002, a survey of 456 US dermatologists found that 23% of respondents used dermoscopy.22 An additional survey in the same year showed that 51% of dermatology program directors incorporated dermoscopy training in their programs.23 In 2009, 48% of responding members of the American Academy of Dermatology endorsed the use of dermoscopy in their practice24 and a later survey study found that 100% of responding program directors trained their residents in dermoscopy in 2017.25 A study conducted in 2018 in Germany found that 98.4% of respondents used dermoscopy.26 While this data should be interpreted with some caution due to the potential for response bias, it remains clear that the use of dermoscopy has seen an immense rise in popularity.
Part of this popularity results from studies which have demonstrated that the use of dermoscopy improves sensitivity and specificity of diagnosing both melanocytic and keratinocytic skin cancers compared to visual inspection alone.1,2 However, the continued rise in prevalence is likely due to multiple additional factors including improvements in speed, efficiency, cost, and overall quality of dermatoscopes, along with a growing list of indications and capabilities. For example, the use of dermoscopy has been increasing in the context of general dermatological disorders including inflammatory dermatoses, pigmentary dermatoses, infectious dermatoses, and disorders of the hair, scalp, and nails.4 Modern terms to describe these indications include: pigmentaroscopy for pigmented lesions, trichoscopy for the scalp and hair, onychoscopy for nails, inflammoscopy for inflammatory dermatoses, as well as entomodermoscopy of skin infestations and infections.4,27 Moreover, there are numerous extra-diagnostic indications for this technique. Evaluation of disease activity in alopecia areata and vitiligo have led to improvements in disease management.28,29 Aesthetic dermatology has benefited from dermoscopy with enhanced categorization and evaluation of enlarged facial open pores and optimization of outcomes for laser hair reduction.30,31Additionally, patient-doctor relationships have been known to benefit from dermoscopy. For example, one author has demonstrated that patients who refuse investigation of suspicious lesions may decide to pursue a biopsy after being shown malignant features under dermoscopy.32
Current State of the Art
Several modern dermatoscopes offer unique benefits. Most allow users to toggle between nonpolarized light and polarized light, providing detailed visualization of both superficial and deeper structures, respectively. Other important factors to consider with modern day dermoscopy include smartphone compatibility, magnification, charge time, size, and cost. Several manufactures make a wide variety of dermatoscopes to accommodate individuals’ specific needs. Figures 3-5 compare the Heine Delta 30, the DermLite DL4, and the Casio DZ-S50.
Conclusion
Dermoscopy has unveiled a new dimension of fascinating and important skin morphology. From its humble beginnings, this technique has undergone a meteoric rise in popularity and continues to expand its role in patient care. As a testament to its well-studied diagnostic utility, dermoscopy has experienced near universal adoption by dermatologists in the U.S. Still, it serves as an adjunctive tool best used in combination with the macro clinical picture and histopathology to be conclusive. In the future, artificial intelligence and computer-assisted diagnosis may aid in the diagnostic capabilities of dermoscopy as these modalities have already been well studied and show great promise.33
Funding Sources
No funding sources were secured for this study.
Disclosures
Dr. Lio reports research grants/funding from the National Eczema Association, AOBiome, Regeneron/Sanofi Genzyme, and AbbVie; is on the speaker’s bureau for Regeneron/Sanofi Genzyme, Pfizer, Eli Lilly, LEO, Galderma, and L’Oreal; reports consulting/advisory boards for Almirall, ASLAN Pharmaceuticals, Dermavant, Regeneron/Sanofi Genzyme, Pfizer, LEO Pharmaceuticals, AbbVie, Eli Lilly, Micreos, L’Oreal, Pierre-Fabre, Johnson & Johnson, Level Ex, Unilever, Menlo Therapeutics, Theraplex, IntraDerm, Exeltis, AOBiome, Realm Therapeutics, Altus Labs (stock options), Galderma, Amyris, Bodewell and My-Or Diagnostics.
Joe Dodson reports no conflict of interest.