Introduction
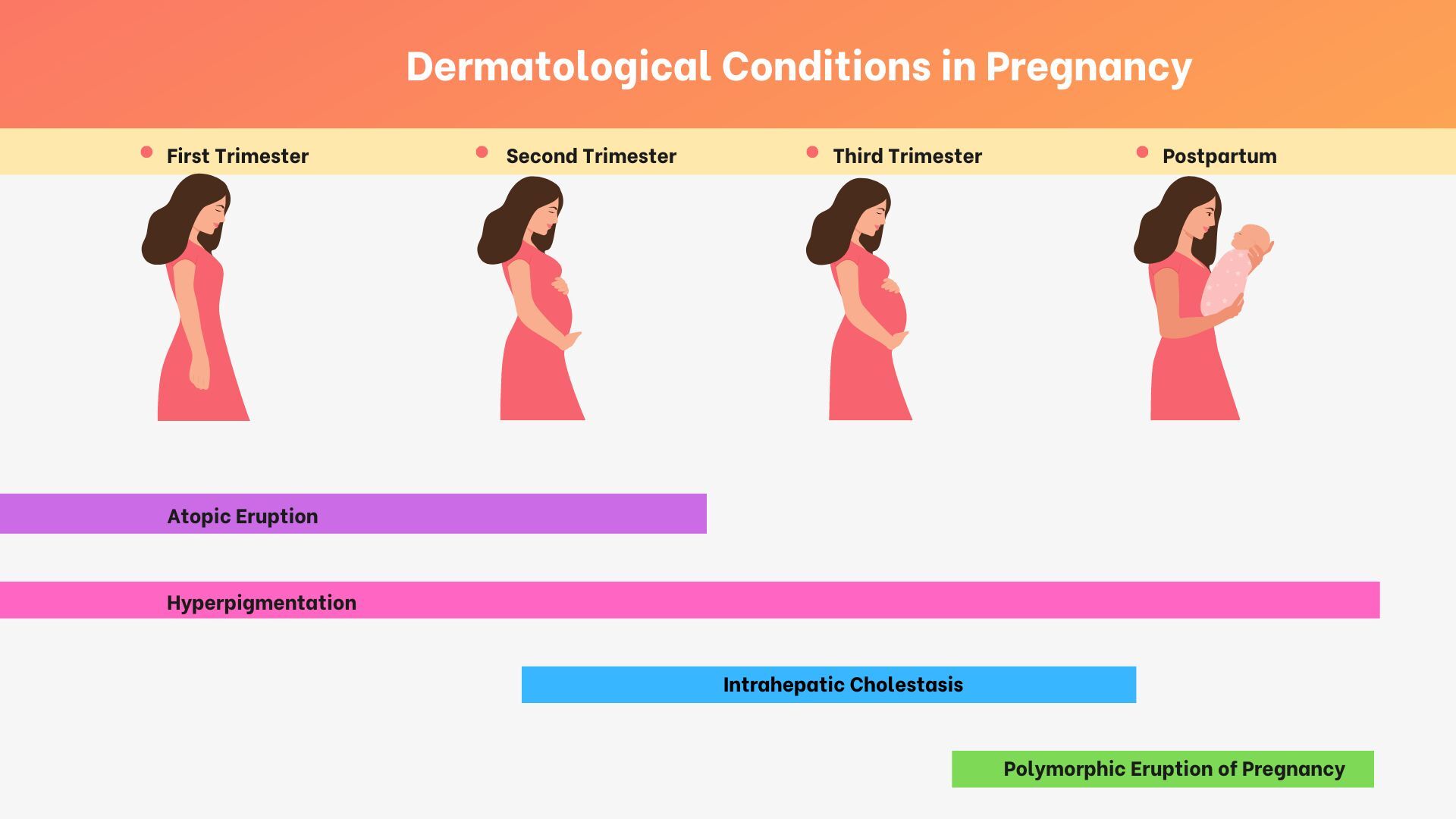
The skin changes vastly during pregnancy.1 While not completely understood, a complex interplay between metabolism, immunology, and hormones is involved leading to many dermatologic metamorphoses.2 Pregnancy leads to the development of many gestational-specific dermatological disorders, including the atopic eruption of pregnancy, polymorphic eruption of pregnancy, pemphigoid gestationis, and intrahepatic cholestasis of pregnancy.3 (Figure 1)
Pruritus remains the most common and troublesome symptom of these pregnancy-related conditions.3 Holistic treatment for these conditions has recently gained attention as integrative approaches broaden the possibilities for symptomatic relief to the mother while limiting possible harm to the fetus.3 In this review, we discuss pruritus-related disorders of pregnancy and integrative treatment.
Conditions related to pruritus in pregnancy
Pruritus in pregnancy is extremely common, affecting nearly 20% of all pregnant women.1,3 There are several pregnancy-specific pruritic diseases, including the atopic eruption of pregnancy, polymorphic eruption of pregnancy, pemphigoid gestationis, and intrahepatic cholestasis of pregnancy.3,4 Aside from these specific disorders, a new dermatosis coinciding with pregnancy is still possible.3 Though pruritus is such a prevalent symptom in pregnancy, it is often underrated by physicians, and data regarding the safety profiles of drugs for pruritus is lacking.3
Atopic dermatitis of pregnancy
The pathogenesis of atopic eruption during pregnancy is not wholly understood.3,5–7 Similar to traditional atopic dermatitis, atopic dermatitis of pregnancy is also thought to be a Th2-mediated disease.3,5–7 Atopic exacerbation of pregnancy typically appears earlier than other pregnancy-related dermatoses.3,5–7 While atopic dermatitis of pregnancy itself is not associated with adverse fetal outcomes, the child might be at risk of developing atopic dermatitis, and the mother can develop atopic dermatitis of pregnancy in subsequent pregnancies.3,5–7 Finally, pregnant women suffering from atopic dermatitis should be aware of the possibility of viral and bacterial infections due to the possibility of many infectious agents crossing the placenta and posing fetal harm.
Polymorphic eruption of pregnancy
Polymorphic eruption of pregnancy (PEP), also known as pruritic urticarial papules and plaques of pregnancy, is a benign self-limiting pruritic inflammatory disorder with an incidence of 1:120-1:300 pregnancies.3,8–10 This disorder typically presents in the third trimester of pregnancy or immediately postpartum.3,8–10 Pregnant women with PEP usually present with highly pruritic urticarial papules that coalesce into plaques, small vesicles 1-2 mm in size (without bullae), widespread non-urticated erythema, and targetoid and eczematous lesions that generally spare the periumbilical region.3,8–10 In contrast to atopic dermatitis of pregnancy that can recur in subsequent pregnancies, PEP rarely recurs and poses no harm to the mother or baby.3,8–10
Intrahepatic cholestasis
Intrahepatic cholestasis of pregnancy (ICP) is a liver disorder solely seen in pregnancy with strong epidemiologic components.3,11–13 ICP most commonly occurs in South American and Northern European ethnic groups and in women with multiple gestations, advanced maternal age, conception with in-vitro fertilization, hepatitis C infection, and a positive family history of ICP.11–14 ICP usually presents in the second or third trimester with severe pruritus classically starting on the palms and soles from the elevated levels of bile acids.3,11–14 Most importantly, ICP has a negative influence on the fetus.3,11–13 Fetal outcomes associated with ICP include preterm birth, stillbirth, respiratory distress, and meconium-stained amniotic fluid.11–13 Maternal complications of ICP aside from pruritus include right upper quadrant pain, nausea, poor appetite, mild jaundice, sleep deprivation, steatorrhea, and vitamin K deficiency.11–14 ICP recurrence is common and similar to pemphigoid gestationis; when this disorder recurs, it occurs at an earlier gestational age with greater severity.11–14
Pustular psoriasis of pregnancy
Pustular psoriasis of pregnancy (PPP) can be a life-threatening condition for both the mother and baby.15–17 Though debate exists over the classification of this disease, PPP usually occurs in the third trimester and is characterized by widespread coalescent pustules and desquamation.15–17 In contrast to many dermatoses of pregnancy, PPP has severe systemic symptoms, including fever, neutrophilia, diarrhea, delirium, electrolyte abnormalities, and elevated inflammatory markers.15–17 Skin changes typically begin with the formation of sterile cutaneous pustules in the skin folds that spread centrifugally while sparing the face, palms, and soles.15–17
Conventional approach to pruritus in pregnancy
Conventional treatment approach to pruritus in pregnancy focuses on treating the underlying disorder and can include antihistamines, glucocorticosteroids, immunosuppressants, and biologics.3,4 In early pregnancy, the first-generation H1 (sedating) anti-histamine chlorpheniramine (4 mg every 4-6 hours) is often used as these are classified as FDA pregnancy category B.3,18–20 While second-generation antihistamines are non-sedating and have fewer side effects than first-generation antihistamines, the introduction of these agents in the first trimester can result in fetal malformations including neural tube defects, hypoplastic left heart syndrome, and teratology of Fallot.3,18–20 Therefore, second-generation antihistamines should be introduced from the second trimester onwards; levocetirizine was a category B drug, while fexofenadine was a category C drug.3,18–20
Phototherapy with narrowband UVB is a second-line treatment for pruritus in pregnancy, especially in early pregnancy when mothers cannot use other drugs.3,21,22 Although there is no direct link between exposure to high levels of UVB radiation and delivery outcomes, there is a lack of studies on light therapy and maternal and fetal effects.3,21,22 There is an increased risk of developing melasma with UV exposure, so patients should be advised to wear a facial covering.3,21,22
Topical glucocorticosteroids are generally safe for pregnancy and may be used for pruritus relief.23–25 Large-scale population studies and meta-analyses have found no increased risk of newborns being born prematurely, underweight, or with any orofacial defects irrespective of the topical glucocorticosteroid potency and amount used.24–26 However, further studies are warranted to provide further evidence for other fetal outcomes.24 Additionally, the effectiveness and safety of drug regimens in pregnancy have not been studied, such as the Aron regimen which comprises topical steroid, mupirocin, and a moisturizer base compounded together.27
If pruritus does not respond to phototherapy or topical steroids and mandates a prolonged course of systemic glucocorticosteroids, steroid-sparing agents, including cyclosporine, or as a final resort, azathioprine can be considered.3,4,28 Cyclosporine is an FDA pregnancy category C drug, while azathioprine was classified as a category D drug, so should be used only by an experienced clinician in this context.3,29,30 Though the studies determining the teratogenicity of these drugs did not investigate the use of these drugs in dermatological conditions, reported outcomes indicated adverse fetal events, including low body weight, premature labor, heart defects, and intrauterine growth restriction.3,29,30
In patients refractory to antihistamines, omalizumab, a humanized recombinant monoclonal antibody that binds to the IgE heavy chain, is believed to be a safe and effective therapeutic modality in pregnant patients.3,31,32 The anti-IL-4 receptor antibody dupilumab is highly successful in treating refractory atopic dermatitis.3,33,34 Though there have not been any reported adverse outcomes with this drug in pregnancy, there are only limited case reports with successful maternal fetal results, so caution should be implemented in using this drug in pregnancy until more data regarding the safety profile of this drug is available.3,33,34
Integrative approach to pruritus in pregnancy
First and foremost, because of the severity and difficulty of treating pruritus in pregnancy, a collaboration between all providers is essential, including dermatologist, gynecologist, midwife, and general practitioner.3 Other integrative approaches, including acupuncture, cupping, vitamin C, aromatherapy, and massages, can be considered.35
Several studies have demonstrated that acupuncture can improve symptoms and quality of life in patients with pruritus.35–37 A possible mechanism for itch reduction by acupuncture in patients with atopic dermatitis is the reduction of in-vitro allergen-induced basophil activation and modulation of brain areas involved in itch processing, such as the insula and putamen.35 Additionally, acupuncture may also modulate neurotransmitters and peripheral hormone levels such as beta-endorphin, adrenocorticotrophic hormone, and somatostatin.35 Finally, acupuncture is considered safe in pregnancy, posing no risks to the mother or fetus.38
Cupping is a part of traditional Chinese medicine that involves placing bamboo or glass cups on a patient’s skin by creating negative pressure inside the cups.35 Cupping therapy can reduce the symptoms of pruritus and is primarily safe in pregnancy, with care to be taken to avoid cupping the lower and upper abdomen, cupping the lower back only till the sixth month of pregnancy, and using light or medium cupping methods only.35,39,40
While no studies have examined aromatherapy’s effects on pruritus in pregnant women, aromatherapy has been shown to improve symptoms of uremic-pruritus and pruritus and stress in older women.35,41,42 Additionally, as aromatherapy may reduce pain symptoms in labor,36 aromatherapy for pruritus in pregnancy could be considered.
Meditation and mindfulness are other important modalities to consider for pruritus in pregnancy. Mindfulness refers to the act of consciously trying to stay in the present moment, which can be expressed through meditation.43 Both meditation and mindfulness have been found to be successful in reducing symptoms of atopic dermatitis and providing other benefits including anxiety reduction.43 Additionally, meditation is safe in pregnancy and has demonstrated stress reduction in expectant mothers.44
Quercetin is a flavonoid that binds to histamine receptors to decrease pruritus and inflammation.45 While quercetin has not been extensively studied in the pregnant population, rodent studies show that fetal quercetin consumption in-utero may lead to liver abnormalities later in life.46 However, some studies still recommend pregnant women consume fruits high in quercetin because of quercetin’s possible role in mediating cardiac disease.47 Therefore, the role of quercetin in pregnancy is still controversial and remains undecided.
N-acetyl cysteine is a compound typically used to treat acetaminophen overdose as it is a strong antioxidant. However, N-acetyl cysteine may offer numerous benefits in pregnancy by reducing apoptosis and free-radical damage.48–50 Furthermore, N-acetyl cysteine has proven to be worthwhile in decreasing excoriations.51 Thus, N-acetyl cysteine should seriously be considered for pruritus in pregnancy, especially in women with skin-picking symptoms.
Hydrogels are an upcoming area of research. While hydrogels for pruritus have not specifically been studied in pregnancy, hydrogels show great promise in treating pruritus in atopic dermatitis.52 Additionally, while the composition of various hydrogels can differ, hydrogels seem to be safe overall in pregnancy as studies are underway investigating hydrogels in the role of endometrial repair and cervical insufficiency.53,54
Even though there are no compelling studies evaluating the role of massages in mitigating symptoms of atopic dermatitis,55 massage therapy has been shown to reduce pruritus in patients with chronic kidney disease56 and adolescents managing burn-induced pruritus.35 Massage therapy may also help with the pain of labor and delivery36; thus, massage therapy for pruritus in pregnancy could be considered. Finally, topical vitamin C is another treatment modality that can improve pruritus in pregnancy, serves various neurobiological functions to both the mother and the fetus, and most importantly, is safe to use.57–59 (Table 1).
In conclusion, various factors contribute to physiological skin changes in pregnancy.1,2 Some of these factors include metabolism, immunology, and hormone alteration.2 While many conventional treatments are safe to use in pregnancy, studies have shown success with an integrative approach to treat pruritus in pregnancy.35–37,40,57,58,60–64 Though the development of many pregnancy-specific dermatoses is unknown, integrative treatment, collaboration between providers, and patient education offer numerous benefits.3,35,65,66
Funding Sources
No funding sources were secured for this study.
Disclosures
Dr. Lio reports research grants/funding from the National Eczema Association, AOBiome, Regeneron/Sanofi Genzyme, and AbbVie; is on the speaker’s bureau for Regeneron/Sanofi Genzyme, Pfizer, Eli Lilly, LEO, Galderma, and L’Oréal; reports consulting/advisory boards for Almirall, ASLAN Pharmaceuticals, Dermavant, Regeneron/Sanofi Genzyme, Pfizer, LEO Pharmaceuticals, AbbVie, Eli Lilly, Micreos, L’Oréal, Pierre-Fabre, Johnson & Johnson, Level Ex, Unilever, Menlo Therapeutics, Theraplex, IntraDerm, Exeltis, AOBiome, Realm Therapeutics, Altus Labs (stock options), Galderma, Amyris, Bodewell and My-Or Diagnostics.
KA reports no conflict of interest.